
Top
Search
People also search for:
- Home
- DevOps for Healthcare Platforms: Automating Compliance & Deployment

Healthcare is undergoing a deep and lasting digital transformation. Patient portals, telemedicine, remote monitoring devices, electronic health records, clinical decision support systems, and AI-driven diagnostics are now core to modern care delivery. When software deployment was delayed, a patient had to wait for critical test results, delaying timely diagnosis and treatment decisions.
To avoid such scenarios, these systems must be delivered quickly, reliably, and critically secure. The complexity of healthcare environments, the sensitivity of protected health information (PHI), and the strict regulatory landscape make traditional manual release processes untenable.
On average, manual releases can cost healthcare institutions upwards of $100,000 annually in inefficiencies and extended downtimes. Additionally, penalties for data breaches stemming from inefficient processes can reach millions, underscoring the need for more agile, secure methodologies.
DevOps for healthcare answers this need by merging development and operations with security and compliance through automation and continuous delivery. When designed specifically for healthcare, DevOps helps teams automate compliance checks, reduce human error, accelerate deployments, and keep platforms auditable and resilient.
This article explains how DevOps transforms healthcare platform delivery, outlines the technical and operational building blocks, and provides a practical roadmap for implementing DevOps automation in regulated healthcare environments.
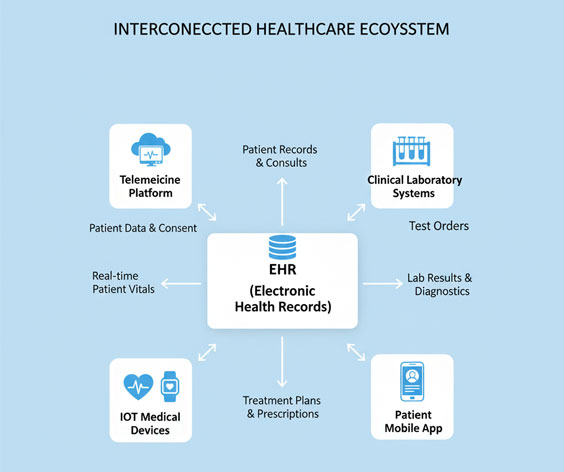
Healthcare platforms must simultaneously satisfy competing priorities. They must protect patient privacy to meet regulations such as HIPAA and GDPR. They must be highly available because downtime can directly impact patient care.
They must interoperate with legacy systems, third-party labs, devices, and payer systems. And they must evolve quickly to support new clinical workflows or respond to security vulnerabilities.
Because of these constraints, every change to a healthcare platform carries substantial risk. Manual compliance checks, ad-hoc deployments, and brittle integration testing amplify that risk.
Healthcare DevOps addresses this by embedding compliance into software pipelines, codifying environment behavior, and automating verifiable audit evidence. The result is faster yet safer delivery: teams can push critical fixes or features without compromising patient safety or regulatory posture.
Manual processes are slow and inconsistent. They rely heavily on human rigor, and humans make errors, especially under time pressure. Automation reduces risk by eliminating repetitive human steps, consistently enforcing policies, and producing immutable evidence that auditors can review. Automation also accelerates time-to-market for features that benefit patients and clinicians.
Automating deployment and compliance does not mean removing human oversight. It means shifting human effort to higher-value activities—designing controls, reviewing automated evidence, and focusing on patient outcomes—while letting machines perform routine enforcement and verification.
In practice, DevOps compliance in healthcare embeds policy-as-code into CI/CD pipelines, ensures infrastructure-as-code (IaC) reproducibility, and maintains audit-ready logs for every change.
A central principle of DevOps is shared responsibility. In healthcare, this means developers, operations, security, and compliance specialists collaborate from the start. When compliance requirements are integrated into feature design rather than tacked on at the end, teams produce software that is compliant by default.
To make this collaboration actionable, teams can either hold daily stand-ups with representatives from compliance and security present or schedule weekly joint threat-modeling sessions. Such rituals help avoid last-minute surprises and foster a culture where safety and speed are complementary priorities.
Translating regulatory controls into executable, testable rules—policy-as-code—lets teams enforce those rules automatically. Policy-as-code can check for required encryption, enforce data residency, validate access controls, and block deployments that violate organizational policies. Automated gates produce machine-readable evidence and reduce the time and effort required for manual audits.
Infrastructure-as-code and containerization deliver reproducible environments. When environments are deterministic, teams can reproduce a production state for debugging or audit, eliminate configuration drift, and ensure testing reflects real-world conditions. These practices make secure healthcare application deployment both reliable and auditable.
DevOps encourages continuous verification—automated tests, security scans, and policy checks run for every change. Observability provides the telemetry, logs, and traces that teams need to detect anomalies, investigate incidents, and demonstrate compliance. Together, these practices support rapid, safe deployments while maintaining visibility and control over live systems.
o build a robust, compliant pipeline for healthcare platforms, consider organizing efforts by maturity levels to prioritize adoption. Begin with foundational elements—continuous integration/continuous deployment (CI/CD) and secure artifact management.
As organizations mature, they can adopt more advanced practices, such as automated policy checks, infrastructure-as-code (IaC), and comprehensive observability. By structuring pipeline components into ‘crawl-walk-run’ stages, leaders can more easily navigate their DevOps journey and reduce the overwhelm for those starting from scratch.
CI is the backbone of rapid, reliable delivery. In healthcare, CI must include not only unit and integration tests but also contract testing for external systems, synthetic-data tests that model clinical workflows, and privacy-aware testing that avoids exposing PHI. Security tests—SAST (static application security testing), dependency vulnerability scanning, and secrets detection—should run automatically. Test environments must be isolated, and synthetic data or robust de-identification techniques must be used.
Automated policy gates prevent noncompliant artifacts from progressing through the pipeline. These gates validate encryption-at-rest, encryption-in-transit, TLS versions, IAM (identity and access management) policies, and resource provisioning rules. Policy-as-code frameworks generate deterministic outputs that auditors can evaluate. When a policy gate fails, the pipeline produces a clear remediation path and records the steps for audit.
IaC tools such as Terraform, CloudFormation, or Pulumi allow teams to provision identical environments across development, staging, and production. IaC templates encode security controls, resource tagging, and default least-privilege settings. They also enable blue/green or canary deployments by spinning up parallel environments to test new releases before exposing them to all users.
Artifact repositories and container registries provide provenance and integrity for build artifacts. Secrets management—through HashiCorp Vault, cloud-based KMS, or similar—keeps credentials out of source control, enables rotation, and provides audit logs for access. Pipelines must retrieve secrets securely at runtime and avoid long-lived, hard-coded credentials.
Comprehensive logging, distributed tracing, and metrics are critical for operational excellence and regulatory evidence. Audit logs must be tamper-evident, retained according to policy, and easy to query during an investigation. Observability systems should correlate alerts with deployment events and include context that helps both engineers and compliance teams understand what changed and why.
Pipeline design in healthcare must strike a careful balance: be fast enough to support frequent releases but thorough enough to meet legal and clinical scrutiny.
Isolate integration, staging, and production pipelines so that each stage enforces appropriate controls. Staging should mirror production as closely as possible, including security posture and data handling policies, to reduce surprises when a change reaches live environments. For highly regulated systems, maintain a long-lived staging environment for compliance validation without touching live patient data.
Some changes—especially those that affect clinical workflows or databases—require human approval. Pipelines should integrate approval gates that record who authorized a change, why, and under what conditions. This preserves governance while keeping the pipeline auditable and rollback-friendly. Human approval should be a deliberative process, not a bottleneck that encourages workarounds.
Beyond unit and integration tests, healthcare pipelines need safety-oriented testing: synthetic scenario testing that mimics patient flows, privacy impact assessments, resiliency tests, and load tests that simulate peak clinical usage. Chaos experiments and failure injection can validate resiliency, but they must be scoped carefully and executed in safe environments before any production attempt.
Security must be an intrinsic part of the pipeline. DevSecOps means running SAST, DAST (dynamic analysis), IAST (interactive testing), dependency scanning, and container image scanning in the CI/CD pipeline. Vulnerabilities should be prioritized by risk and regulatory urgency. Automated patching workflows and vulnerability management systems help teams remediate high-risk findings quickly and demonstrate responsiveness to regulators.
Privacy engineering practices—data minimization, pseudonymization, and tokenization—should be designed into data flows. Where analytics or research require access to datasets, secure enclaves, strict contractual controls, and automated verification, reduce risk.
Operational practices ensure that automated deployments translate into real-world reliability.
Techniques such as blue-green deployments, canary releases, and feature flags reduce blast radius by limiting initial exposure. Progressive rollouts enable teams to validate behavior under live conditions while maintaining the ability to rollback instantly if issues arise.
Planned fault injection in controlled environments validates that the system can tolerate outages and degraded conditions. In healthcare, chaos engineering should start in non-production, progress to limited production with safeguards, and always include automated rollback strategies and monitored safety thresholds.
A prescriptive incident response plan is essential. It should define communication paths to clinical staff, regulators, and customers. Post-incident analysis must be blameless and result in documented remediation and control changes. Each postmortem should produce artifacts that can be shown during a compliance review.
Define realistic service level objectives (SLOs) and use them to drive alerts and operational priorities. Tying monitoring to business and clinical impact ensures teams respond to issues that matter most to patient outcomes. SLO-driven monitoring also helps demonstrate reliability to regulators and stakeholders
Transforming to DevOps in healthcare is a phased journey. An effective roadmap blends quick wins with long-term platform-building.
Begin with a maturity assessment: inventory systems, measure deployment frequency, identify manual, high-risk processes, and map regulatory obligations.
Run small pilots on non-critical services to validate tooling and processes.
Invest in an internal platform team or center of excellence that provides pipeline templates, IaC modules, observability standards, and security integrations.
Track metrics such as deployment frequency, change lead time, mean time to recovery, and compliance-specific measures such as time-to-evidence and the percentage of deployments that produce audit artifacts.
Organizational change fails when leaders focus only on tools or automate poorly governed processes. Avoid the following mistakes:
These trends will make automation more powerful and will raise the bar for continuous compliance and security.
DevOps for healthcare platforms is no longer an optional experiment—it has become a strategic necessity for every organization serious about speed, safety, and compliance.
When hospitals, digital health companies, and care delivery networks streamline operations through automated pipelines, policy-driven governance, and proactive monitoring, they create a technology environment that supports continuous improvement without compromising patient security.
Companies like API DOTS continue helping healthcare teams build these modern DevOps ecosystems with scalable workflows and compliance-ready architectures.
Start with small, high-risk areas, adopt automation where clinical reliability matters most, and expand your DevOps maturity with a strong focus on governance. When implemented thoughtfully, DevOps becomes the engine powering secure, traceable, and continuous innovation—ultimately delivering better outcomes for both healthcare providers and the patients who rely on them.
We bring development and operations together seamlessly.Improving deployment speed, reliability, and infrastructure resilience.
Consult DevOps Experts
I am a full-stack developer specializing in building powerful, user-focused EdTech platforms that enhance modern learning. I develop end-to-end digital solutions that help educators teach more effectively and enable students to learn with clarity, flexibility, and engagement. With expertise across UI/UX, backend architectures, APIs, and scalable cloud systems, I create tools that streamline academic workflows, support personalized learning, and deliver data-driven insights. From schools to EdTech startups, I help teams build smart, secure, and future-ready platforms that transform traditional learning into seamless digital experiences.